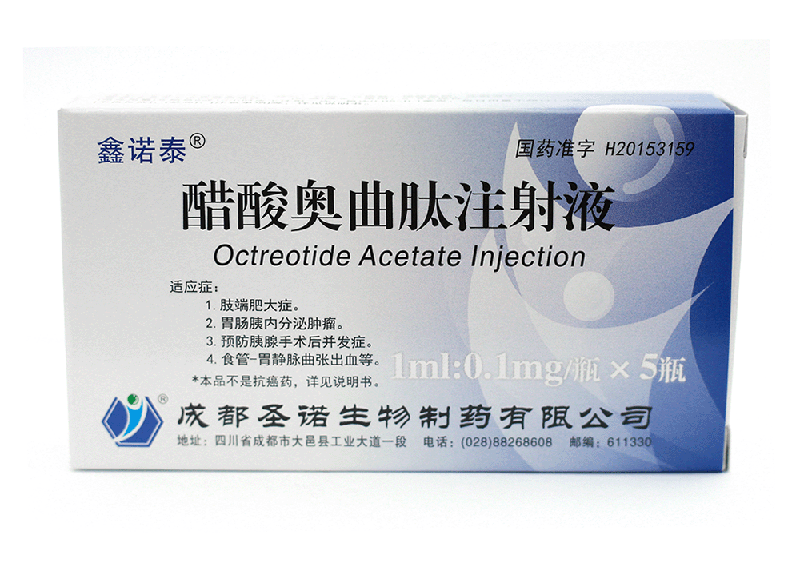
Generic name:OctreotideAcetate Injection
English name:OctreotideAcetate Injection
Pinyin:CusuanAoqutai Zhusheye
【Ingredients】Main ingredients:The main ingredient of this product is octreotide acetate.
Chemical name:Octreotide acetate, d-phenylalanyl-l-cysteyl l-phenylalanyl-l-tryptophenyl l-lysyl-threonyl-n - [(1R
Molecular formula:C49H66N10O10S2.xC2H4O2
molecular weight:1019.26.×60.02
Accessories:Lactic acid, mannitol, sodium bicarbonate, water for injection.
【Character】This product is a clear colorless liquid.
【Indication】 To control the symptoms of acromegaly patients who cannot be adequately controlled by surgical or radiotherapy and to reduce the plasma levels of growth hormone (GH) and insulin-like growth factor-1 (igf-1). Acromegaly patients who are unable or unwilling to undergo surgery may also be treated, or patients with intermittent acromegaly who have not yet been effectively treated with radiotherapy.
[usage and dosage]
acromegaly
Start subcutaneous injection every 8 hours or 12 hours, 0.05-0.1 mg each time, and then make corresponding adjustment according to circulating GH, igf-1 level, clinical reaction and tolerance every month (target: GH less than 2.5 ng/ml; IGF normal range). The optimal daily dose for most patients is 0.2 to 0.3 mg. GH concentrations were measured every 6 months in patients receiving the same dose for a long period of time.
The maximum daily dose shall not exceed 1.5 mg, and the plasma GH level can be reduced as appropriate after several months of treatment by monitoring.
If there is no decrease in GH level and no clinical reaction within 1 month after the treatment, discontinuation should be considered.
Gastrointestinal endocrine tumor
Initially, one or two subcutaneous injections of 0.05 mg/day were administered, gradually increasing to 0.1 ~ 0.2 mg/day three times, depending on the clinical response and the hormone concentration excreted by the tumor (in the case of carcinoid, depending on the excretion of 5-hydroxyindoleacetic acid in urine) and tolerance. Higher doses may be required in individual cases. Maintenance dose varies from individual to individual.
Discontinue medication if clinical symptoms and laboratory tests do not improve within 1 week of administration.
To prevent complications after pancreatic surgery
Subcutaneous injection three times a day, 0.1 mg each time, for 7 consecutive days, the first dose at least 1 hour before surgery.
Esophagogastric varicose bleeding
Continuous intravenous drip of 0.025 mg/h for up to 5 days. Octreotide can be diluted with saline.
In cirrhosis patients with esophagogastric varicose bleeding, octreotide can be given continuous intravenous drip for 5 days at 0.05 mg/h.
Dosage for special patients
Liver insufficiency
In patients with cirrhosis, the half-life of the drug is prolonged, so the maintenance dose needs to be changed.
Renal insufficiency
Renal dysfunction has no effect on total exposure (AUC) after subcutaneous administration, so the dosage of octreotide does not need to be adjusted.
[adverse reactions]
The most frequently reported adverse reactions during octreotide therapy included gastrointestinal, neurological, hepatobiliary, and metabolic and nutritional disorders.
The most common adverse reactions to octreotide in clinical trials were diarrhea, abdominal pain, nausea, flatulence, headache, cholelithiasis, hyperglycemia, and constipation. Other common adverse reactions are dizziness, local pain, biliary sludge formation, thyroid dysfunction (such as decreased thyrotropin [TSH], total T4, and free T4), loose stool, impaired glucose tolerance, vomiting, weakness, and hypoglycemia.
Gastrointestinal disease
In rare cases, gastrointestinal adverse reactions may resemble acute intestinal obstruction with progressive abdominal distension, severe epigastric pain, abdominal tenderness, and muscle tension.
The incidence of gastrointestinal adverse events is known to decrease with the duration of continued treatment.
The occurrence of gastrointestinal adverse reactions can be reduced by avoiding meals before and after administration of octreotide acetate subcutaneously, i.e. between meals or before sleeping.
Injection site reaction
Subcutaneous injection site pain, tingling or burning sensation, accompanied by redness and swelling, rarely lasting more than 15 minutes. Local discomfort can be alleviated by bringing the solution to room temperature before injection or by using a concentrated solution to reduce the injection volume.
Metabolic and nutritional diseases
Although increased fat excretion has been detected in the stool, there is no evidence that long-term use of octreotide causes malnutrition due to poor absorption.
The pancreas
In very rare cases, acute pancreatitis has been reported hours or days prior to subcutaneous treatment with octreotide acetate and recovery after discontinuation. In addition, patients who have been treated subcutaneously with octreotide acetate have reported pancreatitis due to cholelithiasis.
Heart disease.
In patients with acromegaly and carcinoid syndrome, ECG changes such as QT interval extension, electrical axis deviation, early repolarization, low voltage, R/S conversion, early increase of R wave and non-specific st-t wave changes were observed. The association between these events and octreotide acetate has not been established, as most of these patients have underlying heart disease (see [cautions]].
List of adverse reactions in clinical studies
Adverse reactions to octreotide in clinical studies are listed in table 1.
Adverse drug reactions were sorted by frequency using the following criteria: very common (1/10), common (1/100, <1/10), rare (1/1,000, <1/100), rare (1/10,000, <1/1,000), and very rare (<1/10,000), including individual reports. Adverse reactions were ranked in descending order of severity in each frequency group.